Rural communities have different health care needs and challenges than their urban counterparts. A greater proportion of rural patients are elderly, and tend to have high blood pressure and other chronic conditions. Rural residents have less access to medical specialists and mental health workers.
NOTE: Understanding the role culture plays in health care is essential. Still, patients are individuals – each person’s preferences, practices, and health outcomes are shaped by many factors, a concept known as intersectionality.

Rural Minnesotans
Approximately 2,101,500 Minnesotans live in rural areas, accounting for 39 percent of the state’s population. No single definition of rural is used. The majority of residents in rural Minnesota are white (>90%) and were born in Minnesota, although racial and ethnic diversity is increasing (see map). In 1980, only one county had 10 percent or more people of color. In 2010, 18 non-metro counties exceeded 10 percent or more people of color, including four counties at 20 percent or more. Once declining in population, some rural Minnesota counties have seen growth with increasing Latino and African immigrant populations. Eleven percent of all immigrants residing in Minnesota live in rural communities.
Rural communities are older than urban areas, with 44 percent of residents over the age of 50 and 26 percent over 65. More than 1 in 20 residents in rural and small-town areas are 80 years or older, and this proportion is expected to continue increasing.
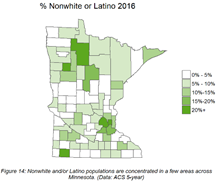 In rural Minnesota, non-white and Latino populations are concentrated in areas such as Willmar, St. Cloud, Worthington, and Rochester. Counties in northern Minnesota have higher percentages of non-white populations due to larger American Indian populations. In addition to English, various other languages may be spoken by these populations.
In rural Minnesota, non-white and Latino populations are concentrated in areas such as Willmar, St. Cloud, Worthington, and Rochester. Counties in northern Minnesota have higher percentages of non-white populations due to larger American Indian populations. In addition to English, various other languages may be spoken by these populations.
- Interpreter Roster: Spoken Language, Health Care, Minnesota Department of Health
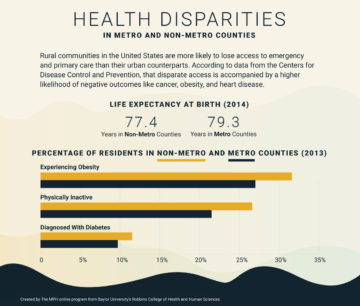
Rural Minnesotans face several disparities in health outcomes and care delivery. Compared to urban areas in Minnesota, rural areas had:
- More people who reported “fair” or “poor” health
- More people who reported being current smokers
- More people who were identified as obese
- Fewer people who reported exercising in the previous month
- Higher mortality rates due to pneumonia and influenza, especially in the older population
- Higher diabetes, stroke, and heart disease mortality rates
- Higher suicide rates
- Higher mortality due to motor vehicle injury.
Rural Minnesotans face several disparities in health outcomes and care delivery.
A Minnesota transportation study found that rural drivers engage in riskier behavior, such as seatbelt noncompliance and driving under the influence (DUI), than urban drivers because they have lower perceptions of the risks associated with these actions.
Rural Minnesotans had better outcomes for some health topics compared to urban residents. They had lower rates of chlamydia, gonorrhea, and HIV/AIDS infection, as well as lower homicide rates. More data on disparities in health and health care for rural Minnesotans:
- Dying Too Soon: County-level Disparities in Premature Death by Rurality, Race, and Ethnicity. University of Minnesota Rural Health Research Center, 2019. (5-page PDF)
- Rural-Urban Differences In Severe Maternal Morbidity And Mortality In The US, 2007–15. Health Affairs, 2019.
- Snapshot of Health in Rural Minnesota. This report provides a snapshot of the health of rural Minnesotans by summarizing key health indicators, health behaviors, and other social and environmental health determinants. Minnesota Department of Health, Office of Rural Health and Primary Care, 2017. (35-page PDF)
 Social determinants of health are economic and social conditions that influence the health of people and communities. Rural residents are more likely to be unemployed, have lower rates of post-secondary education, and have lower median household incomes than urban residents. Those who have health insurance pay a greater percentage of their income in out-of-pocket health care costs.
Social determinants of health are economic and social conditions that influence the health of people and communities. Rural residents are more likely to be unemployed, have lower rates of post-secondary education, and have lower median household incomes than urban residents. Those who have health insurance pay a greater percentage of their income in out-of-pocket health care costs.
- $43,460 was the per capita income for rural Minnesotans compared to $52,038 for the state overall, 2016.
- 11.5 percent of rural Minnesotans live in poverty, compared to 8.9 percent in urban areas, 2017.
- 9.2 percent of rural Minnesota residents did not complete high school, compared to 6.8 percent of the urban population, 2012-2016.
- The unemployment rate in rural Minnesota is 4.2 percent, compared to 3.2 percent in urban Minnesota, 2017.
- More people were uninsured in rural versus urban areas, 2017.
- The 10 counties with the highest teen birth rates are all in greater Minnesota, 2017.
More social determinants impacting rural Minnesotans:
- Health Care Access in Rural Minnesota, Minnesota Department of Health, April 2017. (9-page PDF)
- Rural Health Care in Minnesota: Data Highlights Chartbook, 2019—Chart Summaries. Covers a range of data, including rates of poverty, health insurance coverage, access to health care services, and prescription opioid use. Minnesota Department of Health, Office of Rural Health and Primary Care, 2019.
Though mass media creates a strong American mainstream culture, rural Minnesota populations are culturally diverse. Some of the diversity stems from where communities fit within the continuum of rural. Minnesota has smaller cities (15,000-50,000 people), small towns (less than 15,000 people), and 33 of Minnesota’s 87 counties meet the “frontier” criterion (<6 people/square mile). A rural population’s social structure may be shaped by its dominant economies, such as agriculture, forestry, manufacturing, mining, and tourism.
Traditional rural culture is described as having an importance of family, strong sense of independence, a connection to the land or place, conservatism, influence of faith, use of informal networks, a strong work ethic, and a tendency to value social norms and traditional roles which can be difficult for those who do not fit in to them.
Rural people may experience isolation and a lack of privacy simultaneously. Geographic distance between neighbors may limit time spent with others, resulting in a lack of social support, and creating a barrier to receiving health care or community supports when needed. Fewer people to associate with may result in the sense that everyone knows everything about one another and a stronger feeling of the need to conform or not express opinions that are not conventional, such as sexual orientation and religious or political beliefs.
- Rural Culture is a Diversity Issue. Minnesota Psychologist, January 2004. (4-page PDF)
Many rural communities are food deserts, but rural residents report eating more fruit and vegetables per day than people in urban areas. More people are obese in rural Minnesota than in urban areas, 35.7 percent of the population compared to 28.4 percent.
Rural Minnesotans face shortages of health care providers of all types. Telemedicine is increasingly being used to fill gaps in care delivery. Transportation is an ongoing obstacle for accessing medical care. Rural areas generally had a higher percentage of residents using sliding-fee scales, free or public health clinics. In 2015, a lower percentage of people in rural areas were without a usual source of care, such as a primary provider or clinic, than in past years. This is a key indicator of access to services and whether a person is likely to experience continuity of care.
Independence and self-reliance are survival values for people who live at distances from services and other people. Anonymity and confidentiality are concerns for some rural patients, whether it’s teens accessing sexual health services or people receiving cancer treatment. These barriers may contribute to increased avoidance of seeking health care.
Approximately one in five of all adults in the U.S. experiences mental illness in a given year. Suicide is the second-leading cause of death among people ages 15 to 34 in rural areas. Several factors contribute to fewer people in rural areas seeking and receiving mental health treatment:
- Sparse populations
- Stigma of mental illness
- Long distances that create transportation difficulties
- Lack of service providers
Immigrants and refugees are a growing part of Greater Minnesota’s population. Many live with mental health issues as a result of experienced trauma. Anxiety, clinical depression, and post-traumatic stress disorder (PTSD) are the most common, especially for those who faced cultural destruction and genocide and were forced to flee their homeland. The effects of historical trauma are being studied.
- The Impact of Discrimination. Stress in American, American Psychological Association, 2015.
The five leading causes of death in Minnesota overall are the same in rural areas: cancer, heart disease, unintentional injury, chronic lower respiratory disease, and stroke. Death rates from chronic diseases are higher in rural areas than in urban areas.
When discussing end of life issues with any patient, health care providers need to understand preferences based on personal and family views. People in rural areas are less likely to use hospice and on average spend fewer days in intensive care units than their urban counterparts.
- Rural Palliative Care Resource Center. Resources for communities to improve advance care planning, symptom management, communication, coordination, and delivery of care for those with chronic diseases or life-limiting illness. Stratis Health
Other Populations in Minnesota
African American | American Indian | Asian Indian | Bhutanese | Cambodian | Deaf / Hard of Hearing | Ethiopian | European American | Latinx | Hmong | Iraqi | Karen | LGBTQ | Liberian | Poverty | Rural | Russian | Somali | Vietnamese
